Cvs Caremark Prior Auth Appeal Form . • the patient has a diagnosis of type 2. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. cvs/caremark denial of prior authorization appeal process. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. Appeals for denial of prior authorization for a prescription drug by. the requested drug will be covered with prior authorization when the following criteria are met: the requested drug will be covered with prior authorization when the following criteria are met: • the requested drug will be used with a. a cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s prescription. When a pa is needed for a prescription, the member will be asked to. formulary exception/prior authorization request form. By checking this box and signing.
from exobjyvlx.blob.core.windows.net
the requested drug will be covered with prior authorization when the following criteria are met: • the requested drug will be used with a. • the patient has a diagnosis of type 2. By checking this box and signing. cvs/caremark denial of prior authorization appeal process. Appeals for denial of prior authorization for a prescription drug by. the requested drug will be covered with prior authorization when the following criteria are met: a cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s prescription. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. formulary exception/prior authorization request form.
Cvs Caremark Prior Auth Forms Pdf at Milly Hicks blog
Cvs Caremark Prior Auth Appeal Form the requested drug will be covered with prior authorization when the following criteria are met: Appeals for denial of prior authorization for a prescription drug by. By checking this box and signing. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. • the patient has a diagnosis of type 2. cvs/caremark denial of prior authorization appeal process. the requested drug will be covered with prior authorization when the following criteria are met: When a pa is needed for a prescription, the member will be asked to. a cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s prescription. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. formulary exception/prior authorization request form. the requested drug will be covered with prior authorization when the following criteria are met: • the requested drug will be used with a.
From www.pdffiller.com
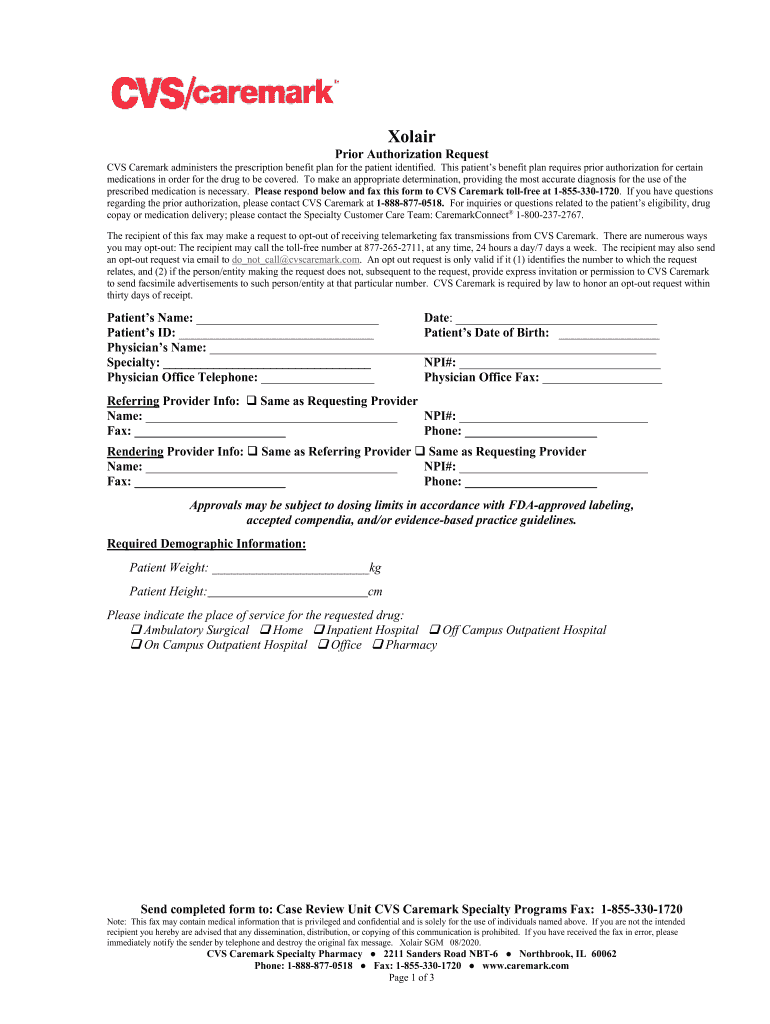
Fillable Online Cvs Caremark Prior Authorization Form Fax Email Print Cvs Caremark Prior Auth Appeal Form to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. the requested drug will be covered with prior authorization when the following criteria are met: Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. • the patient has a diagnosis of type 2.. Cvs Caremark Prior Auth Appeal Form.
From cemvnnwp.blob.core.windows.net
Cvs Caremark Appeal Request Form at Natalie Barker blog Cvs Caremark Prior Auth Appeal Form Appeals for denial of prior authorization for a prescription drug by. By checking this box and signing. cvs/caremark denial of prior authorization appeal process. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. formulary exception/prior authorization request form. • the requested drug will be used with a. . Cvs Caremark Prior Auth Appeal Form.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Auth Appeal Form Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. When a pa is needed for a prescription, the member will be asked to. By checking this box and signing. • the patient has a diagnosis of type 2. cvs/caremark denial of prior authorization appeal process. the requested drug will be covered. Cvs Caremark Prior Auth Appeal Form.
From www.signnow.com
Cvs Caremark Appeal PDF 20032024 Form Fill Out and Sign Printable Cvs Caremark Prior Auth Appeal Form • the requested drug will be used with a. Appeals for denial of prior authorization for a prescription drug by. • the patient has a diagnosis of type 2. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. formulary exception/prior authorization request form. When a pa is needed for a prescription, the. Cvs Caremark Prior Auth Appeal Form.
From exobjyvlx.blob.core.windows.net
Cvs Caremark Prior Auth Forms Pdf at Milly Hicks blog Cvs Caremark Prior Auth Appeal Form • the patient has a diagnosis of type 2. a cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s prescription. formulary exception/prior authorization request form. By checking this box and signing. to make an appropriate determination, providing the most accurate diagnosis for the use of the. Cvs Caremark Prior Auth Appeal Form.
From www.authorizationform.net
Cvs Pharmacy Prior Authorization Form Cvs Caremark Prior Auth Appeal Form • the patient has a diagnosis of type 2. Appeals for denial of prior authorization for a prescription drug by. the requested drug will be covered with prior authorization when the following criteria are met: formulary exception/prior authorization request form. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication. Cvs Caremark Prior Auth Appeal Form.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Auth Appeal Form By checking this box and signing. cvs/caremark denial of prior authorization appeal process. Appeals for denial of prior authorization for a prescription drug by. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. • the patient has a diagnosis of type 2. the requested drug will be covered. Cvs Caremark Prior Auth Appeal Form.
From www.signnow.com
Cvs Caremark Appeal Form Edit & Share airSlate SignNow Cvs Caremark Prior Auth Appeal Form • the requested drug will be used with a. formulary exception/prior authorization request form. the requested drug will be covered with prior authorization when the following criteria are met: the requested drug will be covered with prior authorization when the following criteria are met: to make an appropriate determination, providing the most accurate diagnosis for the. Cvs Caremark Prior Auth Appeal Form.
From www.formsbank.com
Cvs Aveed Prior Authorization Request Form printable pdf download Cvs Caremark Prior Auth Appeal Form Appeals for denial of prior authorization for a prescription drug by. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. cvs/caremark denial of prior authorization appeal process. formulary exception/prior authorization request form. By checking this box and signing. a cvs/caremark prior authorization form is to be used by a medical. Cvs Caremark Prior Auth Appeal Form.
From mungfali.com
Cvs Caremark Prior Authorization Form For Fill Online, Printable E10 Cvs Caremark Prior Auth Appeal Form • the requested drug will be used with a. a cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s prescription. the requested drug will be covered with prior authorization when the following criteria are met: By checking this box and signing. When a pa is needed for. Cvs Caremark Prior Auth Appeal Form.
From www.formsbank.com
Caremark Prior Authorization Criteria Request Form printable pdf download Cvs Caremark Prior Auth Appeal Form When a pa is needed for a prescription, the member will be asked to. formulary exception/prior authorization request form. the requested drug will be covered with prior authorization when the following criteria are met: a cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s prescription. •. Cvs Caremark Prior Auth Appeal Form.
From exobjyvlx.blob.core.windows.net
Cvs Caremark Prior Auth Forms Pdf at Milly Hicks blog Cvs Caremark Prior Auth Appeal Form • the patient has a diagnosis of type 2. the requested drug will be covered with prior authorization when the following criteria are met: By checking this box and signing. a cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s prescription. cvs/caremark denial of prior authorization. Cvs Caremark Prior Auth Appeal Form.
From formspal.com
Caremark Appeal Form ≡ Fill Out Printable PDF Forms Online Cvs Caremark Prior Auth Appeal Form a cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s prescription. formulary exception/prior authorization request form. the requested drug will be covered with prior authorization when the following criteria are met: When a pa is needed for a prescription, the member will be asked to. . Cvs Caremark Prior Auth Appeal Form.
From www.formsbank.com
Caremark Prior Authorization Criteria Request Form printable pdf download Cvs Caremark Prior Auth Appeal Form the requested drug will be covered with prior authorization when the following criteria are met: • the requested drug will be used with a. the requested drug will be covered with prior authorization when the following criteria are met: a cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a. Cvs Caremark Prior Auth Appeal Form.
From www.sampletemplates.com
FREE 8+ Sample Caremark Prior Authorization Forms in PDF Cvs Caremark Prior Auth Appeal Form By checking this box and signing. • the patient has a diagnosis of type 2. Appeals for denial of prior authorization for a prescription drug by. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. formulary exception/prior authorization request form. the requested drug will be covered with prior authorization when the. Cvs Caremark Prior Auth Appeal Form.
From www.pdffiller.com
Fillable Online Cvs caremark prior authorization form Fax Email Print Cvs Caremark Prior Auth Appeal Form When a pa is needed for a prescription, the member will be asked to. the requested drug will be covered with prior authorization when the following criteria are met: By checking this box and signing. cvs/caremark denial of prior authorization appeal process. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of.. Cvs Caremark Prior Auth Appeal Form.
From www.pdffiller.com
Fillable Online CVS Caremark Prior Authorization Forms Fax Email Print Cvs Caremark Prior Auth Appeal Form the requested drug will be covered with prior authorization when the following criteria are met: a cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s prescription. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. to make an appropriate. Cvs Caremark Prior Auth Appeal Form.
From www.sampletemplates.com
FREE 8+ Sample Caremark Prior Authorization Forms in PDF Cvs Caremark Prior Auth Appeal Form the requested drug will be covered with prior authorization when the following criteria are met: formulary exception/prior authorization request form. the requested drug will be covered with prior authorization when the following criteria are met: a cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s. Cvs Caremark Prior Auth Appeal Form.